Diabetic Retinopathy
Introduction
Diabetic retinopathy, a grave consequence of uncontrolled diabetes, is a condition that imperils vision by damaging the delicate blood vessels of the retina. This article elucidates the intricacies of diabetic retinopathy, examining its origins, symptoms, diagnosis, treatment options, and the pivotal role of early intervention.
Understanding Diabetic Retinopathy
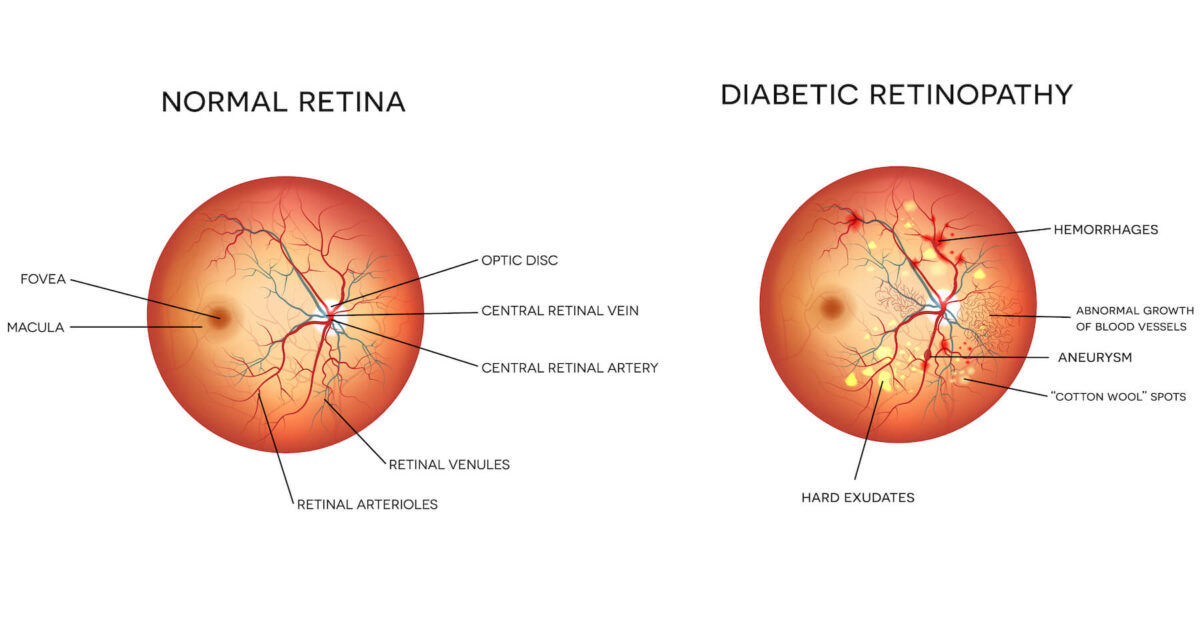
Diabetic retinopathy unfolds when consistently high blood sugar levels impair the small blood vessels nourishing the retina, a crucial part of the eye responsible for vision. As these vessels weaken and leak or become blocked, diabetic retinopathy advances through two stages: non-proliferative and proliferative, each posing unique threats to sight.
Causes and Risk Factors
The chief cause of diabetic retinopathy is diabetes itself, particularly when blood sugar levels remain uncontrolled over time. Several factors heighten the risk of developing this vision-threatening condition, including:
- Duration of Diabetes: The longer one grapples with diabetes, the greater the risk of retinal damage.
- Blood Sugar Management: Consistently elevated blood sugar levels hasten the onset and progression of diabetic retinopathy.
- Blood Pressure: High blood pressure complicates and exacerbates retinal damage.
- Genetics: A family history of the condition increases susceptibility.
- Smoking: Tobacco use magnifies the risk of vision loss in those with diabetes.
Symptoms
In its early stages, diabetic retinopathy may be asymptomatic, underscoring the importance of regular eye exams for individuals with diabetes. As the condition advances, however, it can manifest symptoms such as:
- Blurred or Distorted Vision: Loss of sharpness and clarity in vision.
- Floaters: Tiny specks or cobweb-like structures floating in the field of vision.
- Dark or Empty Spots in Vision: Regions where vision is obscured or absent.
- Impaired Color Perception: Difficulty distinguishing between colors.
- Sudden Vision Loss: A sign of advanced or proliferative diabetic retinopathy.
Diagnosis
Diagnosing diabetic retinopathy hinges on comprehensive eye examinations, which may include:
- Dilated Eye Exam: The eye care professional uses eye drops to enlarge the pupils, allowing for a thorough examination of the retina and its blood vessels.
- Fundus Photography: High-resolution images of the retina are captured to monitor changes over time.
- Optical Coherence Tomography (OCT): This non-invasive imaging test provides cross-sectional images of the retina, revealing abnormalities.
Treatment Options
Managing diabetic retinopathy aims to preserve vision and prevent further damage. Treatment options depend on the stage and severity of the condition and may encompass:
- Laser Photocoagulation: Laser therapy is employed to seal leaking blood vessels or treat abnormal vessel growth.
- Intraocular Injections: Medications are administered into the eye to reduce swelling, leakage, and inflammation.
- Vitrectomy: In cases of advanced bleeding or retinal detachment, a surgical procedure may be necessary to remove blood and scar tissue.
Importance of Early Intervention
The significance of early detection and proactive management of diabetic retinopathy cannot be overstated. Timely intervention not only preserves vision but also reduces the risk of severe complications, including blindness.
Conclusion
Diabetic retinopathy serves as a stark reminder of the critical importance of strict blood sugar control, routine eye examinations, and adherence to recommended treatments. By prioritizing eye health and promptly responding to signs of diabetic retinopathy, individuals with diabetes can aspire to safeguard their vision and enjoy an enhanced quality of life.
