Diabetic Kidney Failure
Introduction
Diabetic kidney failure, medically known as diabetic nephropathy, stands as a formidable complication of diabetes, silently undermining kidney health over time. In this article, we delve into the ominous world of diabetic kidney failure, understanding its origins, the signs it leaves in its wake, methods of diagnosis, available treatments, and the pivotal role of early detection.
Understanding Diabetic Kidney Failure
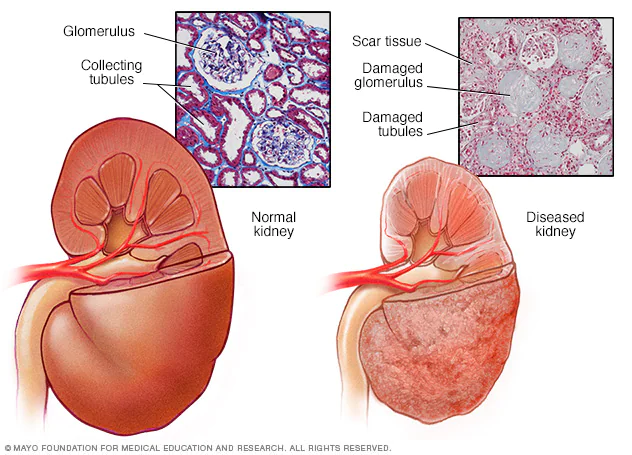
Diabetic kidney failure is the culmination of prolonged damage inflicted on the kidneys by chronic high blood sugar levels, a hallmark of diabetes. This damage manifests as the deterioration of the kidneys’ filtering units, called nephrons. As nephrons falter, the kidneys lose their ability to filter waste products and excess fluids from the bloodstream, setting the stage for a cascade of kidney-related issues.
Causes and Risk Factors
The chief cause of diabetic kidney failure is uncontrolled or poorly managed diabetes. Several risk factors heighten the probability of succumbing to this complication, including:
- Duration of Diabetes: The longer one grapples with diabetes, the more susceptible they become to kidney damage.
- Blood Sugar Mismanagement: Consistently elevated blood sugar levels accelerate the destruction of kidney function.
- Hypertension (High Blood Pressure): Elevated blood pressure compounds the strain on the kidneys.
- Genetic Predisposition: A family history of kidney disease can increase vulnerability.
- Tobacco Usage: Smoking not only worsens kidney damage but also expedites the progression of the disease.
Symptoms
The stealthy nature of diabetic kidney failure means that symptoms may remain elusive until the condition advances. However, as kidney function continues to deteriorate, observable symptoms may emerge, such as:
- Edema (Swelling): Particularly evident in the legs, ankles, and face.
- Fatigue: Unexplained exhaustion and weakness.
- Nocturia: Frequent urination at night.
- Foamy Urine: A telltale sign of excess protein in the urine.
- Elevated Blood Pressure: Often a consequence and contributing factor to kidney failure.
Diagnosis
Diagnosing diabetic kidney failure entails a series of comprehensive evaluations and tests:
- Blood and Urine Tests: To gauge kidney function and assess protein levels in the urine.
- Kidney Biopsy: Occasionally, a small sample of kidney tissue may be extracted for precise damage assessment.
- Imaging Studies: Such as ultrasounds or MRIs to visualize the kidneys and urinary system.
Treatment Options
Managing diabetic kidney failure seeks to halt or slow down the progression of kidney damage while addressing associated complications. Treatment avenues include:
- Blood Sugar Regulation: Rigorous glycemic control is paramount to prevent further kidney deterioration.
- Blood Pressure Control: Medications, lifestyle alterations, and dietary modifications help keep hypertension in check.
- Medications: ACE inhibitors or angiotensin II receptor blockers (ARBs) may be prescribed to safeguard kidney function.
- Dietary Adjustments: Limiting sodium and protein intake may be advised.
- Dialysis: In advanced stages of kidney failure, dialysis may be necessary to replicate kidney filtration functions.
- Kidney Transplant: In severe cases, kidney transplantation may be a viable option.
Importance of Early Intervention
The gravity of diabetic kidney failure underscores the urgency of early detection and proactive management. Timely intervention not only preserves kidney function but also enhances overall quality of life and diminishes the risk of complications such as end-stage renal disease (ESRD) and cardiovascular problems.
Conclusion
Diabetic kidney failure serves as a potent reminder of the profound importance of meticulous blood sugar control, regular medical monitoring, and strict adherence to prescribed treatments. By championing kidney health and responding swiftly to signs of diabetic kidney failure, individuals grappling with diabetes can hope to conserve kidney function and savor an improved quality of life.
