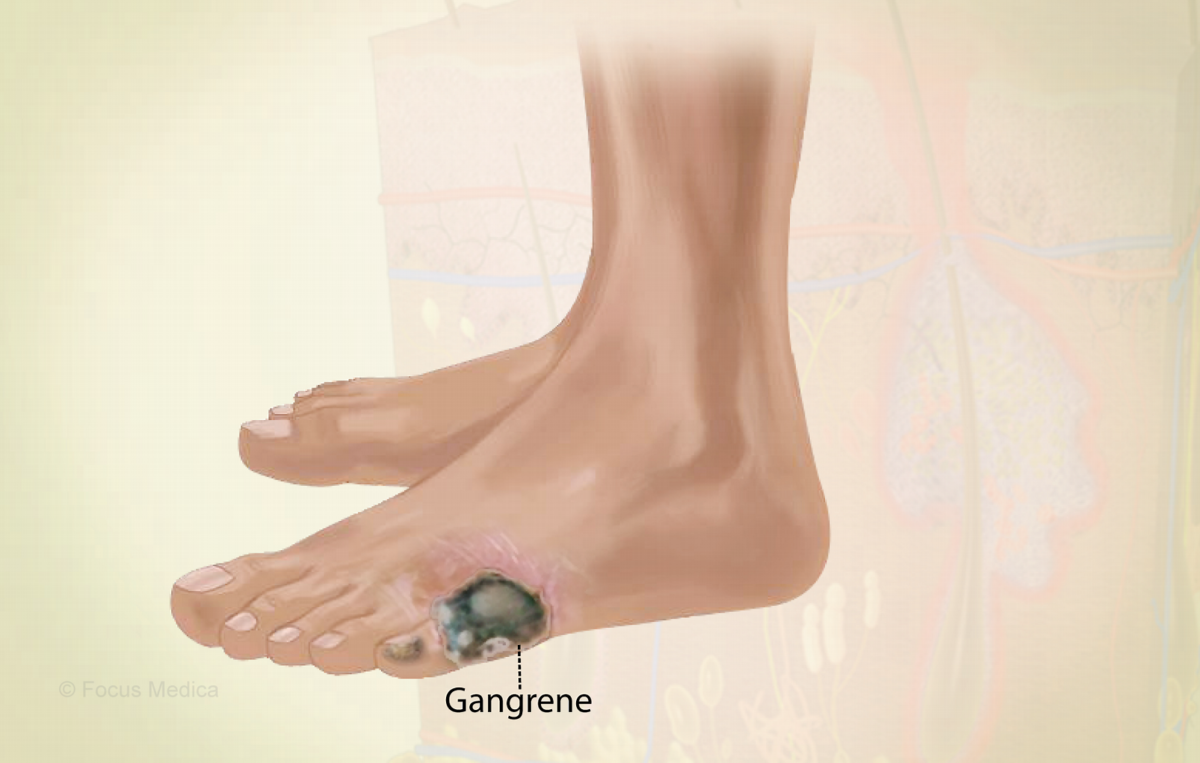
Diabetic Gangrene
Introduction
Diabetic gangrene is a severe and life-threatening complication of diabetes that occurs when high blood sugar levels lead to tissue death and infection. This article explores the ominous world of diabetic gangrene, understanding its origins, signs, diagnosis, treatment options, and the crucial role of prevention and early intervention.
Understanding Diabetic Gangrene
Diabetic gangrene is a result of inadequate blood supply (ischemia) to the extremities, primarily the feet and toes. Prolonged exposure to high blood sugar levels damages the blood vessels and nerves, leading to poor circulation and reduced sensation in the affected areas. As a consequence, minor injuries, ulcers, or infections can progress rapidly, ultimately resulting in tissue death (necrosis) and gangrene.
Causes and Risk Factors
The primary cause of diabetic gangrene is uncontrolled or poorly managed diabetes, particularly when blood sugar levels remain elevated over time. Several factors elevate the risk of developing this life-threatening condition, including:
- Duration of Diabetes: The longer one has diabetes, the higher the risk of tissue damage.
- Poor Blood Sugar Control: Consistently high blood sugar levels hasten the development of gangrene.
- Peripheral Arterial Disease (PAD): Blockages in the arteries that supply the extremities can exacerbate ischemia.
- Peripheral Neuropathy: Nerve damage can dull pain perception, allowing injuries to go unnoticed.
- Smoking: Tobacco use magnifies the risk of gangrene in individuals with diabetes.
Symptoms
Diabetic gangrene can progress rapidly, and its symptoms may include:
- Discoloration: The affected area may turn pale, blue, black, or green.
- Pain: Intense, persistent pain that may precede tissue death.
- Ulcers: Open sores or wounds that do not heal or worsen.
- Blisters: Fluid-filled sacs that may rupture, exposing the underlying necrotic tissue.
- Foul Odor: A characteristic odor emanating from the gangrenous tissue.
- Fever: A sign of infection and systemic illness.
Diagnosis
Diagnosing diabetic gangrene requires a clinical assessment and may involve:
- Physical Examination: A thorough examination of the affected area to evaluate tissue viability and assess for signs of infection.
- Imaging Studies: X-rays, CT scans, or Doppler ultrasound to assess blood flow and identify blockages.
- Tissue Biopsy: In some cases, a sample of the affected tissue may be tested to confirm gangrene and determine the extent of infection.
Treatment Options
Treating diabetic gangrene is an urgent and complex process aimed at preserving life and limb. Treatment modalities may encompass:
- Surgical Debridement: Removal of dead or infected tissue to prevent the spread of infection.
- Antibiotics: Administered to combat infection.
- Revascularization: Surgical or endovascular procedures to restore blood flow to the affected area.
- Hyperbaric Oxygen Therapy: Delivers high-pressure oxygen to enhance tissue healing.
- Amputation: In severe cases, amputation may be necessary to prevent the spread of gangrene and save the patient’s life.
Importance of Prevention and Early Intervention
Preventing diabetic gangrene through meticulous blood sugar control, foot care, and regular medical check-ups is paramount. Recognizing the signs of infection or tissue damage and seeking prompt medical attention can significantly reduce the risk of gangrene and its devastating consequences.
Conclusion
Diabetic gangrene serves as a harrowing reminder of the critical importance of strict blood sugar control, meticulous foot care, and swift response to signs of infection or tissue damage. By prioritizing diabetes management and early intervention, individuals with diabetes can aspire to preserve their limbs and overall quality of life.
