-
Introduction
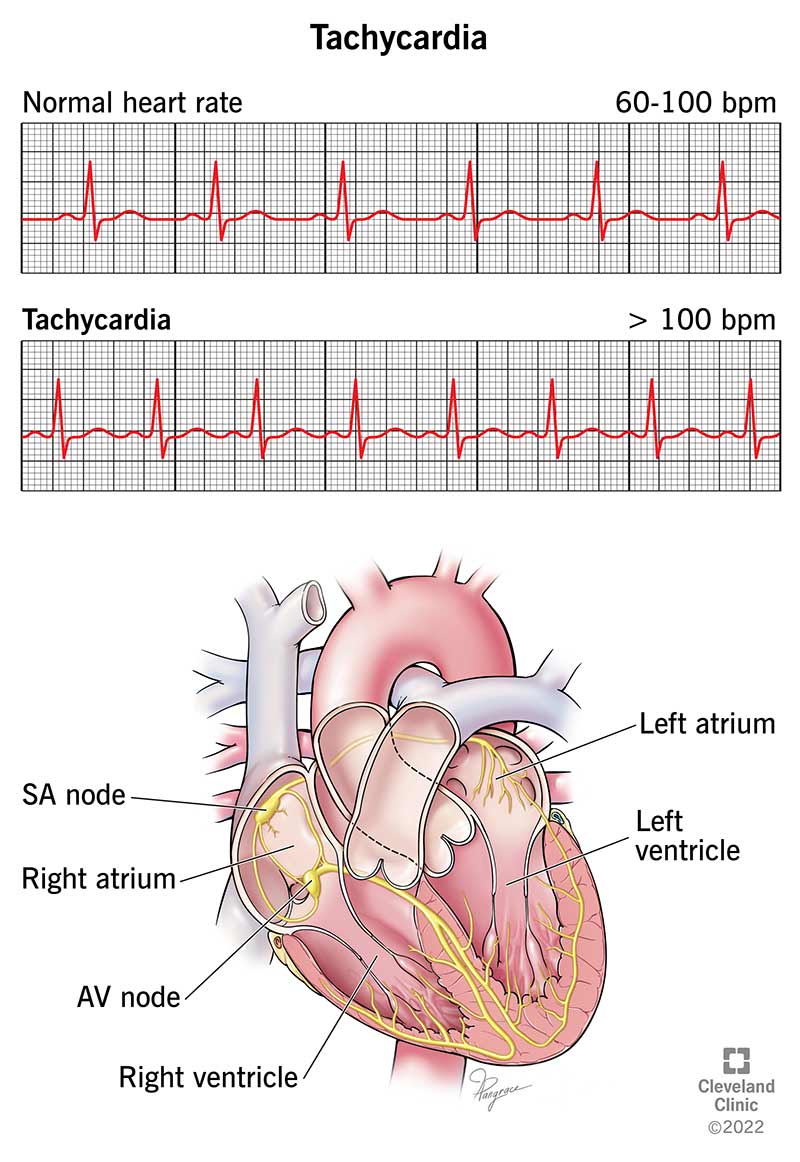
Tachycardia, a medical term describing a faster-than-normal heart rate, is a condition that can affect individuals of all ages. It occurs when the heart beats too quickly, potentially disrupting its normal rhythm and function. This article explores tachycardia, its causes, symptoms, diagnosis, treatment options, and the importance of understanding and managing this condition.
Understanding Tachycardia
Tachycardia refers to a heart rate that exceeds the typical resting rate, which is approximately 60-100 beats per minute (bpm) for most adults. When the heart beats too rapidly, it may not have enough time to fill with blood between contractions, compromising its ability to pump blood effectively. This can lead to a range of symptoms and, in some cases, serious complications.
Causes and Risk Factors
Tachycardia can have various causes, including:
- Stress and Anxiety: Emotional or psychological stress can temporarily increase heart rate.
- Fever: Elevated body temperature can lead to tachycardia.
- Anemia: A reduced number of red blood cells can affect oxygen delivery to tissues and increase heart rate.
- Dehydration: Inadequate fluid levels can result in electrolyte imbalances that affect heart rhythm.
- Heart Conditions: Conditions like atrial fibrillation (AFib), atrial flutter, or ventricular tachycardia can cause rapid heart rates.
- Medications and Stimulants: Certain drugs, caffeine, and stimulants can trigger tachycardia.
- Medical Conditions: Hyperthyroidism, high blood pressure, and heart disease can contribute to tachycardia.
Symptoms
The symptoms of tachycardia can vary depending on the underlying cause and the individual’s overall health. Common symptoms include:
- Palpitations: Feeling a racing, pounding, or fluttering sensation in the chest.
- Dizziness or Lightheadedness: Often accompanied by a feeling of unsteadiness.
- Shortness of Breath: Difficulty breathing, especially during physical activity.
- Chest Pain: Discomfort or pain in the chest, which can be mistaken for a heart attack.
- Fatigue: Unexplained tiredness and weakness.
Diagnosis
Diagnosing tachycardia typically involves a series of tests and evaluations, such as:
- Electrocardiogram (ECG or EKG): Records the heart’s electrical activity, identifying irregular rhythms.
- Holter Monitor: A portable ECG device worn for 24-48 hours to monitor heart rhythms continuously.
- Blood Tests: To check for underlying medical conditions or electrolyte imbalances.
- Exercise Stress Test: Measures heart rate and rhythm during physical activity.
- Echocardiogram: Uses sound waves to visualize the heart’s structure and function.
Treatment Options
The approach to treating tachycardia depends on its cause, severity, and impact on the individual’s quality of life. Treatment options may include:
- Lifestyle Modifications: Managing stress, staying hydrated, and limiting caffeine and alcohol intake.
- Medications: Antiarrhythmic drugs or beta-blockers to control heart rate and rhythm.
- Catheter Ablation: A minimally invasive procedure to treat abnormal electrical pathways in the heart.
- Pacemaker: Implanted to regulate heart rate in certain cases.
- Cardioversion: Electrical shock therapy to restore normal heart rhythm.
Importance of Understanding and Managing Tachycardia
Recognizing the signs of tachycardia and seeking medical attention promptly is crucial. Untreated tachycardia can lead to serious complications, including blood clots, stroke, heart failure, and sudden cardiac arrest. Managing the condition effectively, either through lifestyle changes or medical interventions, can significantly improve the quality of life for individuals with tachycardia.
Conclusion
Tachycardia, characterized by a faster-than-normal heart rate, is a condition that requires attention and appropriate management. Understanding its causes, recognizing symptoms, and seeking medical advice are essential steps toward maintaining a healthy heart rhythm. By doing so, individuals can navigate the challenges of tachycardia and work toward a balanced and heart-healthy life.
CLASSIC LIST
Introduction
Coronary artery narrowing, also known as coronary artery stenosis, is a medical condition where the arteries that supply blood and oxygen to the heart muscle become narrowed or constricted. This condition can impede blood flow to the heart, potentially leading to various heart-related problems. In this article, we delve into coronary artery narrowing, its causes, symptoms, diagnosis, treatment options, and the importance of early intervention.
Understanding Coronary Artery Narrowing
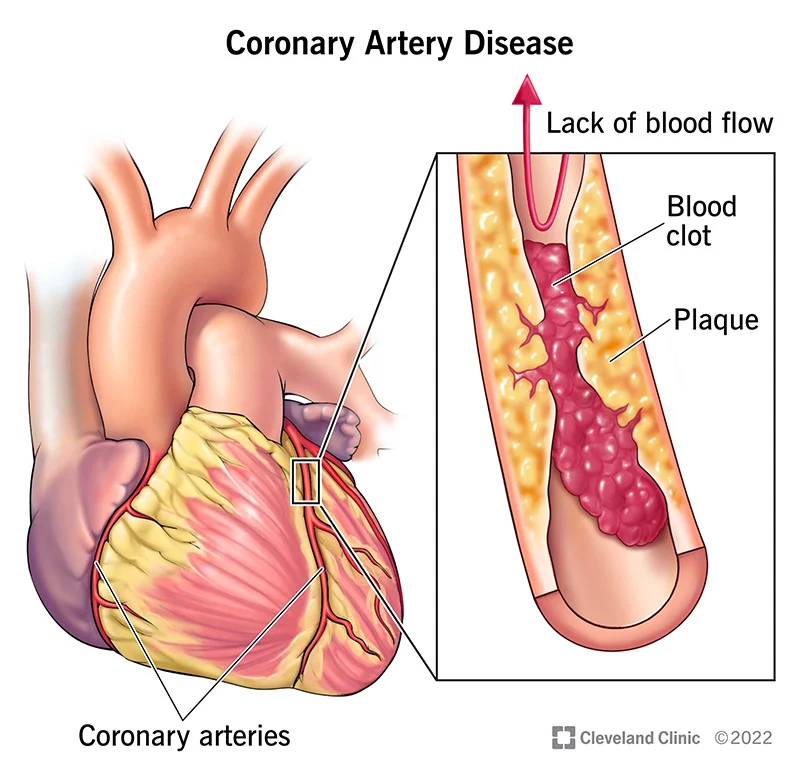
Coronary artery narrowing occurs when fatty deposits, cholesterol, calcium, and other substances accumulate on the inner walls of the coronary arteries, forming plaques. These plaques can gradually reduce the inner diameter of the arteries, restricting blood flow to the heart. This diminished blood supply can result in chest pain (angina), heart attacks, and other cardiac complications.
Causes and Risk Factors
Several factors contribute to the development of coronary artery narrowing, including:
- Atherosclerosis: The primary cause, where plaque buildup occurs over time.
- High Blood Pressure: Hypertension can accelerate the hardening and narrowing of arteries.
- High Cholesterol: Elevated levels of LDL (low-density lipoprotein) cholesterol are associated with increased plaque formation.
- Diabetes: Poorly managed diabetes can damage blood vessels and promote plaque buildup.
- Smoking: Smoking accelerates atherosclerosis and increases the risk of plaque rupture.
- Family History: A genetic predisposition to heart disease can contribute.
- Obesity: Excess body weight increases the risk of developing coronary artery narrowing.
Symptoms
Coronary artery narrowing may not produce noticeable symptoms until it progresses significantly. Common symptoms include:
- Angina: Chest pain or discomfort, often triggered by physical exertion or emotional stress.
- Shortness of Breath: Especially during activity or when lying flat.
- Fatigue: Unexplained tiredness and reduced exercise tolerance.
- Heart Attack: A sudden, severe chest pain that may radiate to the arms, neck, or jaw.
Diagnosis
Diagnosing coronary artery narrowing involves a combination of medical evaluations and tests, including:
- Cardiac Catheterization (Angiography): A procedure that involves injecting contrast dye into the coronary arteries to visualize blockages and assess blood flow.
- Electrocardiogram (ECG or EKG): To detect abnormal heart rhythms or signs of heart damage.
- Stress Testing: Evaluates how well the heart functions under stress, such as during exercise or medication-induced stress.
- CT or MRI Angiography: Non-invasive imaging techniques that can provide detailed views of the coronary arteries.
Treatment Options
The treatment approach for coronary artery narrowing aims to relieve symptoms, improve blood flow, and reduce the risk of complications. Treatment options may include:
- Medications: Statins to lower cholesterol, antiplatelet drugs, and blood pressure medications.
- Lifestyle Modifications: Dietary changes, regular exercise, smoking cessation, and weight management.
- Angioplasty and Stent Placement: A minimally invasive procedure to open narrowed arteries and place stents to keep them open.
- Coronary Artery Bypass Grafting (CABG): In cases of severe narrowing, surgical rerouting of blood flow around blocked arteries may be necessary.
Importance of Early Intervention
Early diagnosis and treatment of coronary artery narrowing are crucial to prevent heart attacks, relieve symptoms, and improve overall heart health. Lifestyle changes and adherence to prescribed medications can significantly reduce the risk of complications associated with this condition.
Conclusion
Coronary artery narrowing is a common cardiovascular condition that can have serious consequences if left untreated. Awareness of risk factors, regular health check-ups, and early intervention are key to managing this condition effectively. Maintaining a healthy heart through a balanced lifestyle and medical care is vital to ensure a long and fulfilling life free from the constraints of coronary artery narrowing.
Introduction
Hypokinesia, often linked to a decreased ejection fraction (EF), is a condition that affects the heart’s ability to pump blood effectively. It’s a medical term that signifies reduced movement or contraction of a specific area, in this case, a portion of the heart muscle. In this article, we delve into hypokinesia, its causes, symptoms, diagnosis, treatment options, and the importance of early intervention.
Understanding Hypokinesia and Decreased EF
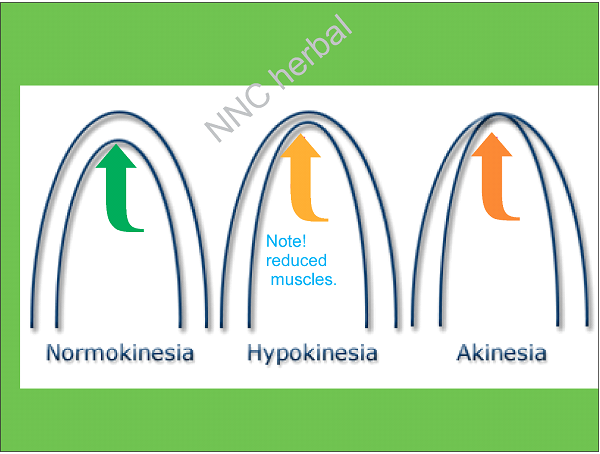
Hypokinesia, in the context of heart health, refers to an area of the heart muscle that contracts less effectively than normal. This decreased contraction can reduce the heart’s pumping efficiency, potentially leading to a reduced ejection fraction (EF). EF is a measure of the heart’s ability to pump blood out of the left ventricle during each beat. A normal EF is typically around 50-70%.
Causes and Risk Factors
Hypokinesia can result from various factors, including:
- Coronary Artery Disease (CAD): Blocked or narrowed coronary arteries can reduce blood flow to parts of the heart muscle, causing hypokinesia.
- Heart Attack (Myocardial Infarction): A heart attack can damage heart tissue and lead to areas of hypokinesia.
- Cardiomyopathy: Conditions that weaken the heart muscle, such as dilated cardiomyopathy or ischemic cardiomyopathy, can cause hypokinesia.
- Hypertension: High blood pressure can lead to hypertrophy (thickening) of the heart muscle, potentially resulting in hypokinesia.
- Valvular Heart Disease: Malfunctioning heart valves can affect blood flow and contribute to hypokinesia.
Symptoms
Hypokinesia itself may not cause noticeable symptoms, but it can lead to symptoms associated with heart failure, such as:
- Fatigue: Feeling unusually tired, even with minimal physical exertion.
- Shortness of Breath: Especially during physical activity or when lying flat.
- Swelling (Edema): Fluid buildup in the legs, ankles, or abdomen.
- Reduced Exercise Tolerance: Difficulty in performing routine activities due to breathlessness or fatigue.
Diagnosis
Hypokinesia and decreased EF are typically diagnosed through a combination of tests and examinations, including:
- Echocardiogram: An ultrasound of the heart that measures EF and identifies areas of hypokinesia.
- Electrocardiogram (ECG or EKG): To assess the heart’s electrical activity and detect irregular rhythms.
- Cardiac MRI or CT Scan: These imaging techniques provide detailed images of the heart, helping to identify the extent and location of hypokinesia.
- Blood Tests: To check for biomarkers associated with heart damage or heart failure.
Treatment Options
Treatment for hypokinesia aims to address the underlying cause and manage symptoms. Options may include:
- Medications: Heart medications, such as beta-blockers, ACE inhibitors, or diuretics, can help manage symptoms and improve heart function.
- Lifestyle Modifications: Dietary changes, exercise, and smoking cessation can improve overall heart health.
- Revascularization: In cases where hypokinesia is due to blocked coronary arteries, procedures like angioplasty and stent placement or coronary artery bypass grafting (CABG) may be recommended.
- Implantable Devices: In severe cases, a cardiac resynchronization therapy (CRT) device or implantable cardioverter-defibrillator (ICD) may be implanted to improve heart function and prevent life-threatening arrhythmias.
Importance of Early Intervention
Early diagnosis and treatment of hypokinesia are vital to prevent further damage to the heart muscle and reduce the risk of complications, including heart failure. Regular follow-ups with a healthcare provider and adherence to prescribed treatments can significantly improve the prognosis for individuals with hypokinesia.
Conclusion
Hypokinesia, often associated with decreased EF, is a condition that affects the heart’s ability to pump blood effectively. We the NNC have herbal formulation containing
Danshen (Salvia miltiorrhiza) is effective herb in cardiac hypokinesia, improves blood in body.
Cayenne Pepper (Capsicum annuum): Cayenne contains capsaicin, which can improve blood circulation and potentially removed hypokinesia.
Ginkgo Biloba: Ginkgo may improve circulation and oxygen delivery to the heart muscle, potentially aiding in the management of cardiac hypokinesia.
Hawthorn (Crataegus): Hawthorn is a well-known herb for supporting heart health. It may help improve blood flow, strengthen the heart muscle, and regulate blood pressure.
Efficacy may be noted just in two weeks.
Introduction
Hypertension, commonly known as high blood pressure, is a widespread health issue that often remains unnoticed until it causes serious complications. Dubbed the “silent killer,” hypertension quietly damages your blood vessels, heart, and other vital organs. This article explores hypertension, its causes, risk factors, symptoms, diagnosis, treatment, and the importance of managing this condition.
Understanding Hypertension
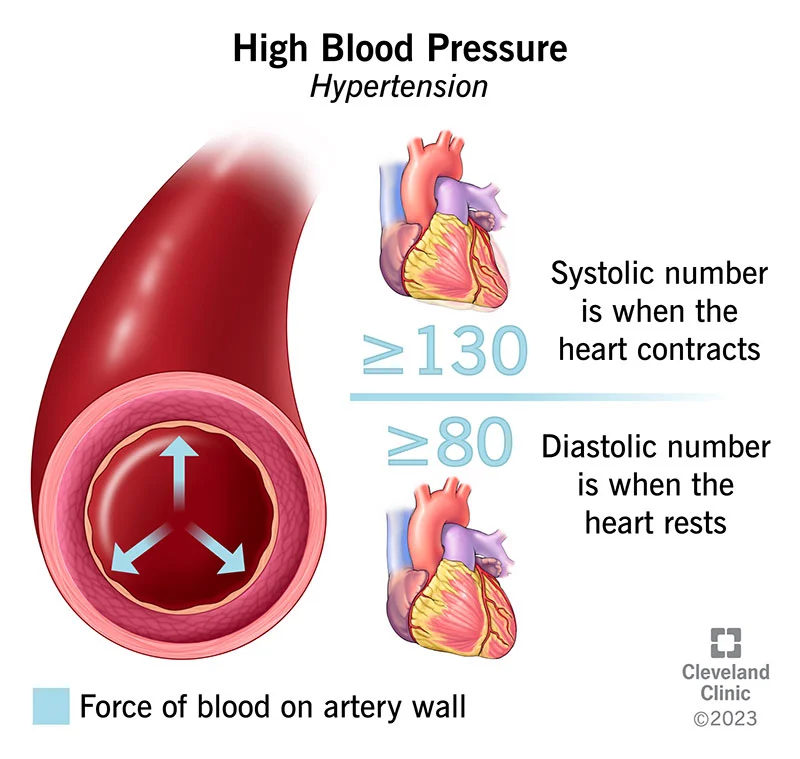
Hypertension is a chronic medical condition characterized by consistently elevated blood pressure levels. Blood pressure is the force of blood against the walls of the arteries as the heart pumps it throughout the body. Two numbers represent blood pressure: systolic pressure (the top number) when the heart contracts, and diastolic pressure (the bottom number) when the heart relaxes. Normal blood pressure is typically around 120/80 mm Hg.
Causes and Risk Factors
The exact cause of hypertension is often unknown, but several factors contribute to its development. Common causes and risk factors include:
- Genetics: A family history of hypertension can increase your risk.
- Unhealthy Lifestyle: Poor diet, lack of physical activity, excessive alcohol consumption, and smoking.
- Age: Hypertension is more common in older adults.
- Obesity: Excess body weight places additional strain on the heart and blood vessels.
- Chronic Conditions: Diabetes, kidney disease, and sleep apnea are associated with high blood pressure.
- Stress: Chronic stress can contribute to elevated blood pressure levels.
Symptoms
Hypertension is often asymptomatic, which is why it’s called the silent killer. Most people with high blood pressure do not experience noticeable symptoms until it reaches a severe stage. In some cases, symptoms may include:
- Headaches: Particularly in the morning.
- Dizziness or Lightheadedness: Especially when standing up.
- Blurred Vision: Occasional vision problems may occur.
- Shortness of Breath: Especially during physical activity.
Diagnosis
Regular blood pressure checks are crucial for early detection. Hypertension is diagnosed based on multiple blood pressure readings taken over time. Diagnosis may involve:
- Blood Pressure Monitoring: Done at a healthcare provider’s office, at home with a blood pressure monitor, or through ambulatory monitoring.
- Physical Examination: To check for signs of target organ damage.
- Laboratory Tests: To identify underlying causes or risk factors.
Treatment Options
Managing hypertension is essential to prevent complications. Treatment approaches include:
- Lifestyle Modifications: Dietary changes (reducing sodium, increasing potassium), regular exercise, weight management, and stress reduction techniques.
- Medications: When lifestyle changes alone are insufficient, doctors may prescribe medications like diuretics, beta-blockers, ACE inhibitors, or calcium channel blockers.
- Regular Monitoring: Frequent check-ups to track blood pressure levels and adjust treatment as needed.
Importance of Management
Controlling hypertension is crucial because unmanaged high blood pressure can lead to serious complications, including heart disease, stroke, kidney problems, and vision impairment. Managing hypertension effectively can significantly reduce the risk of these health issues, improving overall quality of life.
Conclusion
Hypertension is a common and potentially dangerous condition that affects millions of people worldwide. Awareness, early detection, and appropriate management are crucial in preventing its adverse consequences. Making positive lifestyle changes, taking prescribed medications, and adhering to a regular monitoring schedule can help individuals with hypertension take control of their health and reduce the risks associated with high blood pressure. It’s important to note that modern medical science has not defined a cure for high blood pressure, but proactive health management can significantly improve outcomes.
What NNC says?
As above-described basic subject is to change life style to active.
2nd important is food management removed your acid food from menus.
3rd increase alkaline foods.
4th Set your platter at <25% carbs.
5th Increase hepatic and pancreatic enzyme production by changing foods.
6th Have our clinically proven herbal regime containing marjoram, wild Mint and fumaria +
Distilled herbal-waters and specific honey combination.
Stop some bad food permanently – Live without of drugs forever.
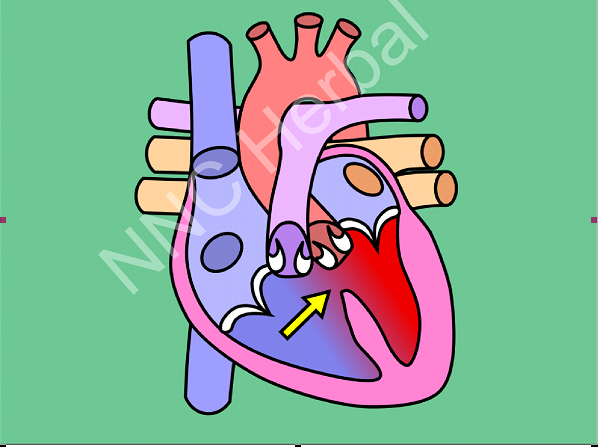
VSD
Treatment Options
The treatment approach for VSD depends on the size and location of the defect, as well as the overall health of the patient. Treatment options may include:
Monitoring: Small VSDs that do not cause symptoms may require only regular checkups to monitor the condition’s progression.
Medications: Medications may be prescribed to manage symptoms, such as diuretics to reduce fluid buildup in the lungs.
Surgery: Large or symptomatic VSDs often require surgical repair. Surgeons can patch or close the hole using various techniques, such as open-heart surgery or minimally invasive procedures.
Catheter Procedures: In some cases, a catheter-based procedure called transcatheter closure may be used to repair the VSD without open-heart surgery.
What NNC says
The Natural Nutrition Clinic (NNC) plays a crucial role in the management of Ventricular Septal Defects (VSDs). With a focus on timely diagnosis and appropriate treatment, NNC strives to achieve over a 65% cure rate for VSDs. Many children who received treatment at our clinic for VSDs have gone on to lead healthy, active, and normal lives. It’s important to note that these positive outcomes are often most significant when the condition is addressed at an early age. Follow-up appointments and external medical opinions are highly recommended to ensure the effectiveness of the treatment.
Our theory is; that VSDs may be linked to imbalances of needed mineral in blood during pregnancy. When VSDs are diagnosed during pregnancy, it can be more manageable to address and complete the septal wall, potentially leading to improved outcomes. At NNC, we apply specific herbal treatments that are rich in essential minerals to support the development and perfection of all cardiac muscles, ultimately aiming to develop septal wall perfectly,
Remarkably, we have observed significant improvements in standard clinical investigations within just 6 weeks of our treatment. These early results indicate the potential for successful management of VSDs through our specialized approach.