Introduction
Loss of sex desire, medically known as hypoactive sexual desire disorder (HSDD), is a complex issue that can be associated with diabetes. This article explores the relationship between diabetes and a diminished libido, understanding the underlying causes, effects on sexual health, coping strategies, and the importance of open communication in addressing this intimate concern.
Understanding Loss of Sex Desire in Diabetes
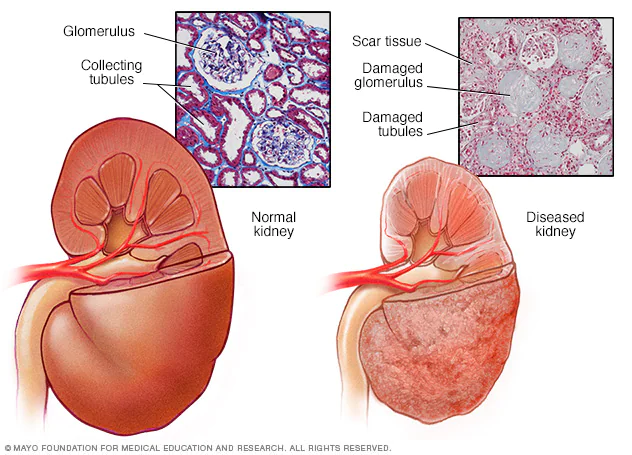
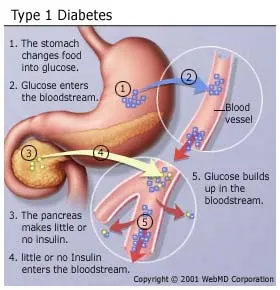
Diabetes is a chronic condition characterized by high blood sugar levels, which can lead to a range of physical and psychological health issues. One of the less-discussed complications of diabetes is its potential impact on sexual health, specifically a reduced desire for sexual activity.
Causes and Risk Factors
Several factors contribute to loss of sex desire in individuals with diabetes, including:
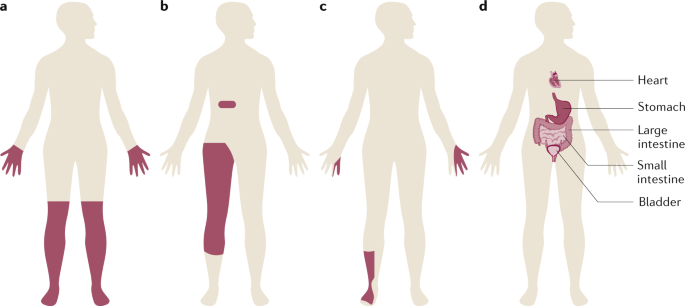
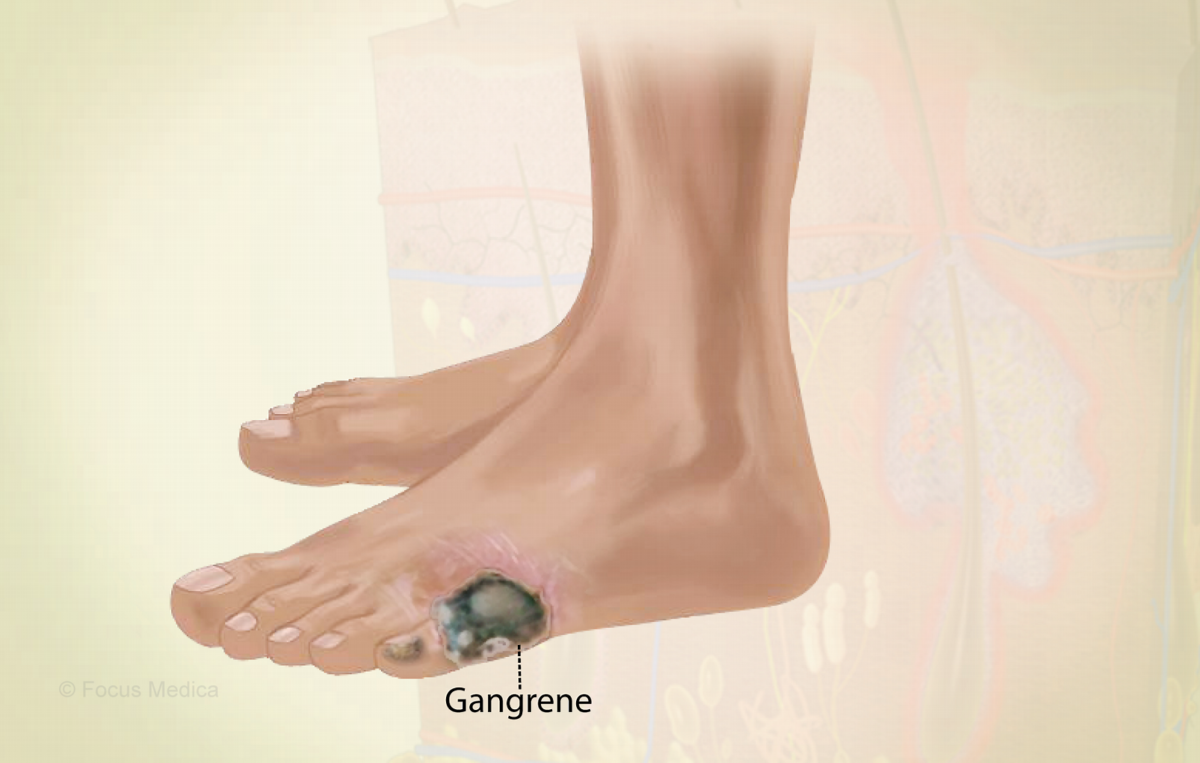
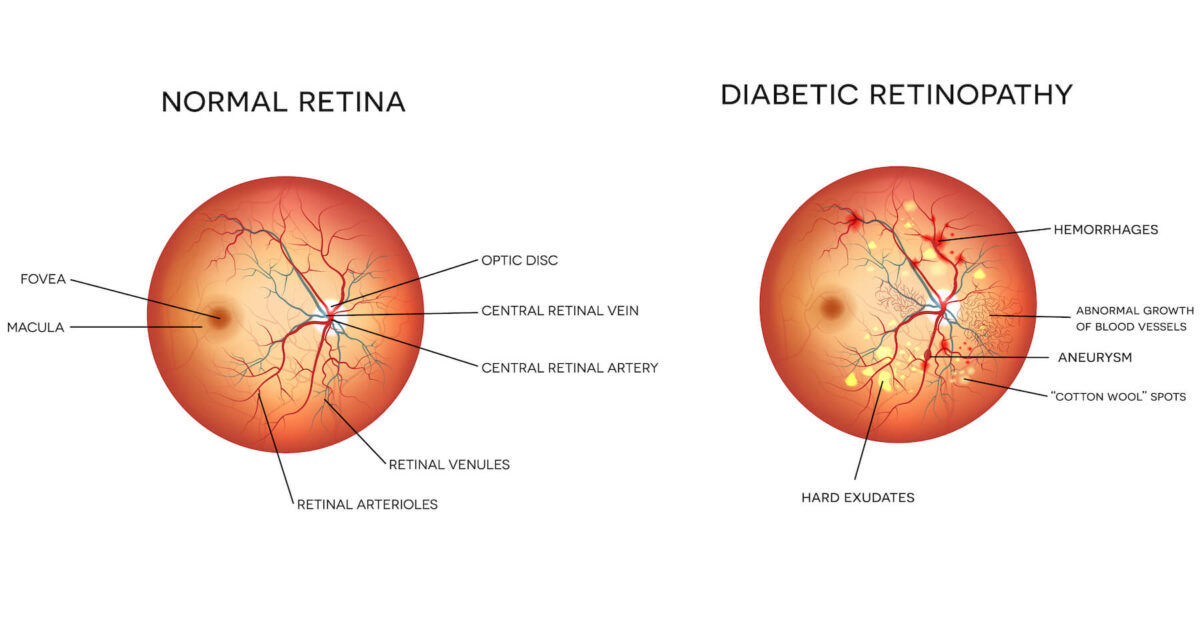
- Physical Factors: Diabetes can damage blood vessels and nerves, affecting blood flow to the genital area and causing sensory changes that impact sexual response.
- Hormonal Imbalances: Diabetes can disrupt hormonal regulation, including sex hormones like testosterone, which plays a crucial role in sexual desire.
- Psychological Factors: The stress, anxiety, and depression often associated with managing diabetes can dampen sexual desire.
- Medications: Some medications used to treat diabetes may have side effects that affect sexual function and desire.
- Relationship Issues: Managing diabetes can place stress on intimate relationships, affecting sexual desire and satisfaction.
Symptoms
The symptoms of loss of sex desire in diabetes can vary from person to person but may include:
- Reduced Interest: A decreased interest or desire for sexual activity.
- Difficulty Becoming Aroused: Difficulty becoming physically aroused or maintaining arousal.
- Pain or Discomfort: Pain or discomfort during sexual activity.
- Emotional Distress: Feelings of frustration, anxiety, or sadness related to changes in sexual desire and function.
Coping Strategies
Managing loss of sex desire in diabetes involves a combination of medical and lifestyle strategies, including:
- Communication: Open and honest communication with your partner is essential in addressing and understanding the issue together.
- Blood Sugar Control: Maintaining good blood sugar control through diet, exercise, and medication can help mitigate the impact of diabetes on sexual health.
- Stress Management: Engaging in stress-reduction techniques such as meditation, yoga, or therapy can help alleviate psychological factors affecting sexual desire.
- Medication Adjustment: Consult with a healthcare provider to discuss medication side effects and potential adjustments.
- Couples Therapy: For individuals in relationships, couples therapy can help improve communication and intimacy.
Importance of Open Communication
Addressing loss of sex desire in diabetes requires open and compassionate communication between partners. It’s crucial to discuss concerns, feelings, and any changes in sexual desire or function openly and without judgment. Seeking support from healthcare professionals or therapists can also be valuable in managing these intimate challenges.
Conclusion
Loss of sex desire in diabetes is a multifaceted issue that can significantly impact an individual’s quality of life and intimate relationships. By understanding the potential causes, seeking medical guidance when needed, and maintaining open communication with partners, individuals with diabetes can work together to address and manage this sensitive concern and maintain a fulfilling and satisfying sexual life.